Recently, a randomized trial comparing elective upper neck irradiation (UNI) versus whole neck irradiation (WNI) in uninvolved neck in patients with nasopharyngeal carcinoma (NPC) was completed by the team of Professors Jun Ma and Ling-Long Tang from Sun Yat-sen University Cancer Center. The results showed similar survival in both groups, but less radiation toxicity and better quality of life in patients receiving UNI. The findings were published in The Lancet Oncology.
NPC is endemic in SouthChina. Cervical lymph node metastasis is common in NPC, and thus prophylactic WNIis currently recommended. In such irradiation modality, the incidence of radiation-relatedtoxicity is high, with 40% of patients developed hypothyroidism within 2 years. The team of ProfessorJun Ma and Ling-Long Tang has been committed to the research of individualizedneck irradiation for NPC. In 2009, the team proposed that lymph node metastasisfollows an orderly pattern in NPC: (1) involving the upper neck drainage areafirst, and then to the lower neck drainage area, with rare skip metastasis; (2)ipsilateral metastasis, with a very low incidence of contralateral metastasis. Basedon these findings, the team performed several retrospective studies which foundthat elective UNI in the uninvolved neck can also provide similar survivalrates as WNI. To provide high-quality evidence, in 2016, this team conducted aprospective, randomized, multicentre phase 3 clinical trial to compare theclinical results of elective UNI versus WNI in the uninvolved neck in NPC.
Methods: NPCPatients with T1-4N0-N1M0 disease (according to the 7th edition of AJCC TNM)were randomly assigned (1:1) to receive elective UNI or WNI for the uninvolvedneck. The primary endpoint was regional relapse-free survival (RRFS).
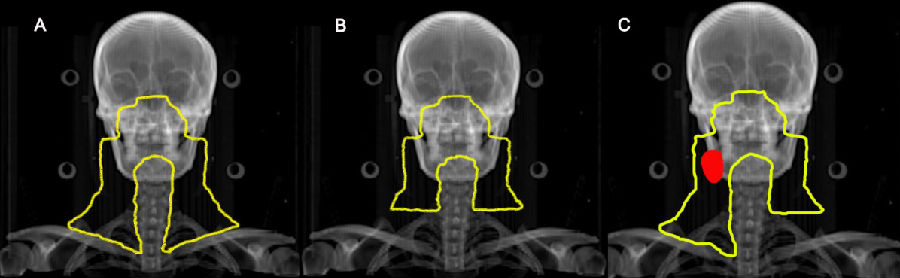
Schematic diagram
A:WNI group:whole neck irradiation, regardlessof the nodal status
B:UNI group:Bilateral upper neck irradiationfor the bilateral uninvolved neck
C:UNI group:Upper neck irradiation for the ipsilateraluninvolved neck, and whole neck irradiation for the involved neck (red areashows the involved lymph node)
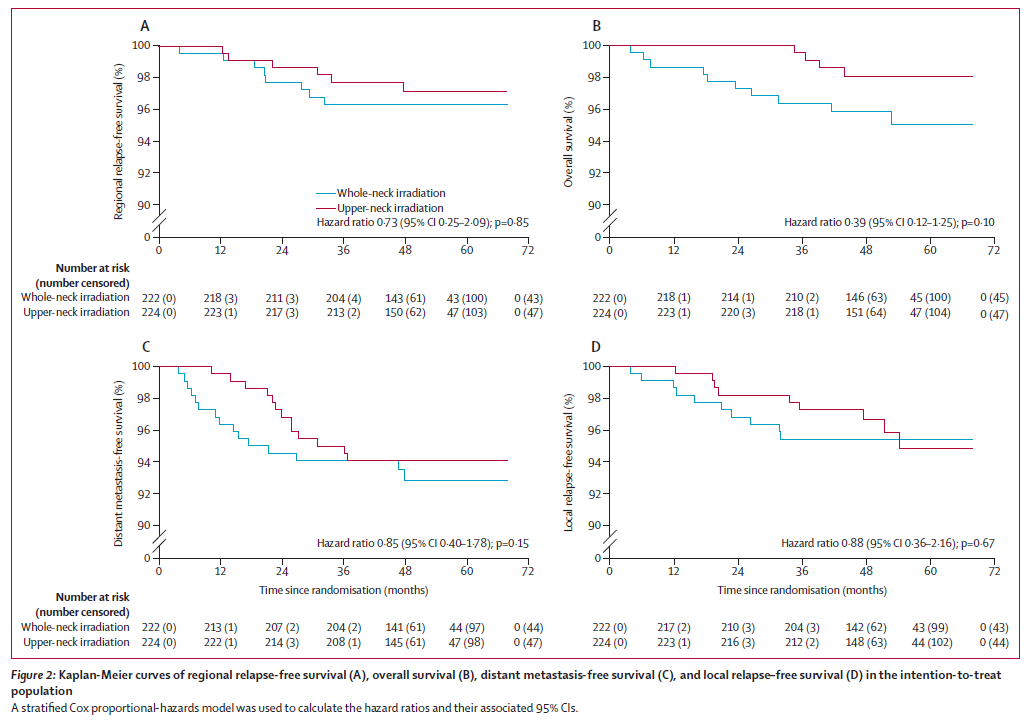
Results: 446patients were enrolled, with a median follow-up of 53 months. 3-year RRFS wassimilar between the UNI and WNI group (97.7% vs 96.3%,pnon-inferiority<0·0001).
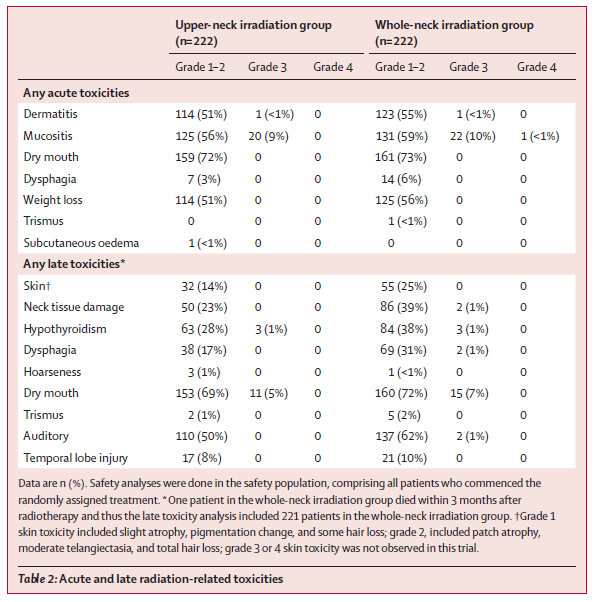
Acute radiation-related toxicities were similar, but UNI group had a lower incidence of late toxicity including hypothyroidism (30% vs. 39%), skin (14% vs. 25%), dysphagia (17% vs. 32%), and neck tissue damage (23% vs. 40%). Moreover, UNI group had statistically better quality of life outcomes, including global health status, emotional functioning, fatigue, and swallowing.
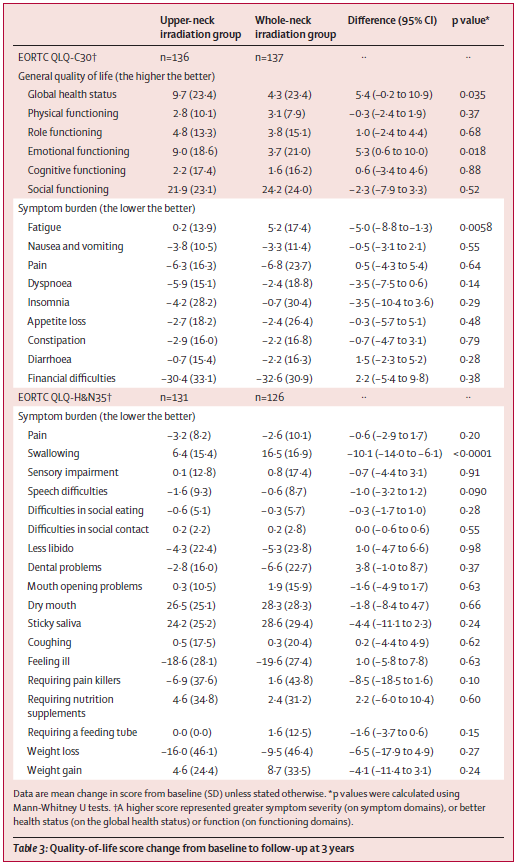
Conclusions: Thisstudy proposes individualized neck irradiation for NPC: for patients withoutcervical lymph node metastasis, the target volume should include only bilateralupper neck (above the cervical cricoid cartilage); for patients with unilateralcervical lymph node metastasis, the target volume should include the bilateralupper neck and the ipsilateral lower neck. Such irradiation modality reducesthe irradiation volume of several organs and structures, provides comparablesurvival, less radiation toxicity, and better quality of life to standard WNIin patients with N0-1 NPC. A considerable number of patients (70%) could bebenefit from this effective and less-toxic treatment, which might rewrite theclinical treatment guidelines of NPC.

Copyright © 1998 - 2026 Chinese Society of Clinical Oncology(CSCO). All Rights Reserved
Contact Us
EMAIL:office@csco.org.cn
international@csco.org.cn
Phone:86(10)67726451 (Beijing)
86(25)84547290 (Nanjing)